To create complex wearable devices, one may make use of one of the Internet of Things designs outlined in this paper.
The fact that wearables are constrained in size and have limited computational power should be noted, as a typical system architecture would include a gateway to the Internet (e.g., a smartphone) with a dedicated application used for configuring the device as well as processing the data received from the device.
- It is also possible to utilize the gateway device for data visualization purposes, in which case relevant processed data is converted into a graphical representation.
- A low power transceiver (e.g., Bluetooth Low Energy (BLE)) is used to transmit the received data wirelessly, which is then processed in the device's memory.
- In the Cloud, data processing is more complete and analytical, allowing for more informed decisions.
- When finished processing, the data is transmitted back to the wearable device for feedback, with a copy of the data being stored in the data center.
- Obviously, the gateway is responsible for establishing network connection in order to facilitate such back-and-forth communication.
Illustration below depicts the architecture of a typical wearable device in terms of its functionality.
It should be emphasized that wearables might be either more or less sophisticated than what is shown, depending on their purpose.
- For example, certain wearable navigators used by professional hikers link directly to a Global Positioning System (GPS), avoiding the gateway layer in the process, and so saving time.
- Some early fitness trackers, on the other hand, relied only on a smartphone for processing and input, eliminating the necessity for a Cloud service.
THE ARCHITECTURE OF WEARABLE IoTS.
Creating a WIoT ecosystem in which body-worn sensors smoothly synchronize data with cloud services via the IoT infrastructure is no longer adequate; rather, it has become critical to construct independent wearable devices in order to succeed in the future.
On top of the IoT architecture is now being developed a revolutionary integrative framework for the Internet of Things (IoT).
The following covers all of the components of the Internet of Things architecture, as well as their interconnections, a system that would be beneficial to the healthcare business in a number of different ways.
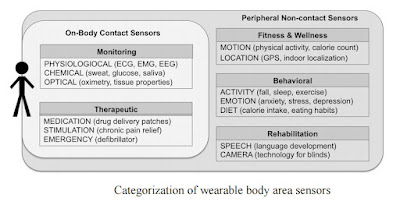
Body Area Sensors.
In the Internet of Things, wearable body area sensors (WBAS) are components that unobtrusively encircle the body in order to collect health-centric data.
WBAS are primarily responsible for,
1) collecting data from the body, either directly from the body through contact sensors or indirectly from the body and its behaviors through peripheral sensors (see illustration above), and
2) preparing the data for either on-board analysis for close-loop feedback or remote transmission for comprehensive analysis and decision support.
WBAS, whether they are commercial products or laboratory prototypes, are bundled with tiny sensor gear, an embedded CPU with storage capabilities, power management, and optional communication circuits, depending on their intended use.
Wearable sensors such as the BodyMedia wristband (Jawbone Inc., USA) are examples of peripheral wearable sensors that function on algorithms that need little computing and just the bare minimum of hardware, with the purpose of encouraging users to keep an active lifestyle.
Because they are needed to give accurate, high-resolution clinical information about patients in real time, the majority of contact-type wearable sensors are equipped with adequate electronics and computational capabilities.
In wearable technology, a novel interface between the sensor and the body is essential for efficient data collecting.
Pulse oximetry using a ring sensor, chest-worn ECG monitor, and attachable BioPatch are only a few examples of innovative sensor sites that provide continuous access to the body's vital signs.
Smart textiles are becoming more popular.
- Smart textiles are at the forefront of wearable electronics that are woven into the fabrics of clothing in order to offer unobtrusive health monitoring for patients who live in their homes, away from hospitals and physicians.
- Smart clothing equipped with textile-based sensors have been proven to be effective in monitoring the reaction of the autonomous nervous system.
Regardless of the end-user applications for which they are designed, WBAS are needed to fulfill worldwide quality standards in order to guarantee that they can operate for an extended period of time with the least amount of monitoring and management.
The need for wearable sensors has prompted the downsizing of technology and the development of energy-efficient methods of lowering power consumption while maintaining clinically acceptable performance criteria.
Researchers continue to face difficulties in managing data from wearable sensors since such data must be tagged with information such as time, activity, and location.
Gateways that are linked to the internet.
Because of their low computational power and connection capacity, WBAS are seldom used as stand-alone systems in today's world.
- As a result, they must transport data to powerful computing resources, which may be either companion devices such as smartphones, tablets, and laptop PCs, or cloud computing servers that are situated in a different location.
- The usage of companion devices as gateway devices is common in both cases of data transfer, and they constitute an essential class of WIoT devices that allow information to flow from sensors to the cloud or server centers for storage and further analysis.
- Wearable sensors exchange data with the Gateway devices through short-range communication technologies such as Bluetooth, while heterogeneous networks such as WIFI and GSM are utilized to deliver the data to the cloud via the Gateway devices.
The ability to retain data, execute certain pre-processing algorithms to determine whether or not the data is clinically relevant, and broadcast the data sporadically to distant servers are all capabilities of some Gateway devices.
Weight scales may transfer data to a mobile smartphone, which then sends the information to a cloud-based server, allowing physicians to analyze weight control in children and adolescents.
Smartphones communicate with cloud servers in order to monitor fall detection in older people.
Examples such as these illustrate how wearable gadgets or other devices used by the user connect with a smartphone or with a phone in order to transmit information to distant servers.
- Mobile Cloud Computing (MCC) is a paradigm that optimizes mobile computing and networking protocols in order to reduce the load of computing on smartphones in order to increase the performance and battery life of smartphones.
- The Internet of Things (IoT) may reap considerable benefits from MCC since it allows for data storage and analysis to take place on cloud platforms.
Support for the Cloud and Big Data.
It is expected that the confluence of intimate companions—wearable sensors and smartphones—will result in an unparalleled influx of medical data into cloud storage facilities.
As crucial as getting information from the body is the process of gaining knowledge from that information.
Patients only profit from wearing sensors when clever algorithms evaluate the data and provide recommendations on what to do as a result of the findings.
A cloud computing infrastructure can make the administration of wearable data easier, as well as supporting sophisticated data mining, machine learning, and medical big data analytics capabilities.
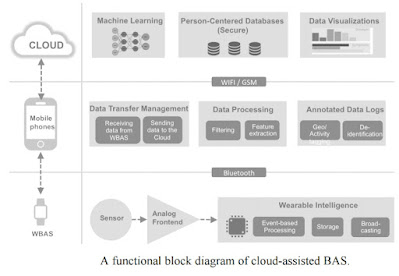
In the next years, the cloud-assisted BAS (CaBAS) will emerge as a promising technology that will enable the integration of MCC and WBAS, hence facilitating the creation of scalable, data-driven ubiquitous healthcare.
CaBAS can provide significant benefits to the Internet of Things, as illustrated in below.
These include,
1) energy-efficient routing protocols that can network smartphones and wearable sensors for handshaking and seamless data transfer,
2) event-based processing that can reduce unwanted data processing on resource-constrained wearable sensors, and
3) annotated data logs that can add activity-level information on top of clinical data for enhancing the accuracy of machine learning algorithms on the Cloud data set.
Find Jai on Twitter | LinkedIn | Instagram
References and Further Reading:
- Asada HH, Shaltis P, Reisner A, Rhee S, Hutchinson RC: Mobile monitoring with wearable photoplethysmographic biosensors. IEEE Eng Med Biol Mag (2003), 22:28-40.
- Batch, Bryan C., et al. "Weight loss intervention for young adults using mobile technology: Design and rationale of a randomized controlled trial—Cell Phone Intervention for You (CITY)." Contemporary clinical trials 37.2 (2014): 333-341.
- G. Yang, et al. "A Health-IoT Platform Based on the Integration of Intelligent Packaging, Unobtrusive Bio-Sensor and Intelligent Medicine Box," IEEE Transactions on Industrial Informatics (TII), doi: 10.1109/TII.2014.2307795, 2014.
- Gubbi, Jayavardhana, et al. "Internet of Things (IoT): A vision, architectural elements, and future directions." Future Generation Computer Systems 29.7 (2013): 1645-1660.
- F. Seoane, et al. “Sensorized Garments and Textrode-Enabled Measurement Instrumentation for Ambulatory Assessment of the Autonomic Nervous System Response in the ATREC Project” vol.13, no.7, pp. 8997-9015, Jul. 2013.
- Fernando, Niroshinie, Seng W. Loke, and Wenny Rahayu. "Mobile cloud computing: A survey." Future Generation Computer Systems 29.1 (2013): 84-106.
- Fortino, Giancarlo, et al. "Bodycloud: a saas approach for community body sensor networks." Future Generation Computer Systems 35 (2014): 62-79.
- Market Study Report, “Wearable Computing Devices, Like Apple’s iWatch, Will Exceed 485 Million Annual Shipments by 2018”, ABI Research. Feb. 21, 2013.
- Mankodiya, K., et al. "Wearable ECG module for long-term recordings using a smartphone processor." Proceedings of the 5th International Workshop on Ubiquitous Health and Wellness, Denmark. 2010.
- Press Release, “FDA Clears NeuroMetrix Wearable Technology for Over-the-Counter Use in Treatment of Chronic Pain”. Jul 18, 2014.
- Sharma, Vinod, et al. "SPARK: Personalized Parkinson Disease Interventions through Synergy between a Smartphone and a Smartwatch." Design, User Experience, and Usability. Springer International Publishing, 2014. 103-114.
- Terry G. Mahn, “Wireless Medical Technologies: Navigating Goverment Regulation in New Medical Age”. A report on medical device regulation. Released on Nov. 2013.
- Zhang, Q., Ren, L., & Shi, W. HONEY: a multimodality fall detection and telecare system. Telemedicine and e-Health, (2013): 19(5), 415-429.